Dissociative identity disorder
| Dissociative Identity Disorder | |
|---|---|
| Classification and external resources | |
| ICD-10 | F44.8 |
| ICD-9 | 300.14 |
| MeSH | D009105 |
Dissociative identity disorder is a psychiatric diagnosis that describes a condition in which a person displays multiple distinct identities or personalities (known as alter egos or alters), each with its own pattern of perceiving and interacting with the environment. In the International Statistical Classification of Diseases and Related Health Problems the name for this diagnosis is multiple personality disorder. In both systems of terminology, the diagnosis requires that at least two personalities routinely take control of the individual's behavior with an associated memory loss that goes beyond normal forgetfulness; in addition, symptoms cannot be the temporary effects of drug use or a general medical condition.[1]
There is a great deal of controversy surrounding the topic. There are many commonly disputed points about DID. These viewpoints critical of DID can be quite varied, with some taking the position that DID does not actually exist as a valid medical diagnosis, and others who think that DID may exist but is either always or usually an adverse side effect of therapy.[2][3][2][4][5][6] DID diagnoses appear to be almost entirely confined to the North American continent; reports from other continents are at significantly lower rates.[7][8]
Contents |
Signs and symptoms
Individuals diagnosed with DID demonstrate a variety of symptoms with wide fluctuations across time; functioning can vary from severe impairment in daily functioning to normal or high abilities. Symptoms can include:[9]
- Multiple mannerisms, attitudes and beliefs that are not similar to each other
- Unexplainable headaches and other body pains
- Distortion or loss of subjective time
- Comorbidity
- Depersonalization
- Derealization
- Severe memory loss
- Depression
- Flashbacks of abuse or trauma
- Unexplainable phobias
- Sudden anger without a justified cause
- Lack of intimacy and personal connections
- Frequent panic/anxiety attacks
- Auditory hallucinations of alternate personalities (though these hallucinations typically posses a quality that makes them distinct from psychotic disorders or schizophrenia)
Patients may experience an extremely broad array of other symptoms that resemble epilepsy, schizophrenia, anxiety disorders, mood disorders, post traumatic stress disorder, personality disorders, and eating disorders.[9]
Physiological findings
Reviews of the literature have discussed the findings of various psychophysiologic investigations of DID.[10][11] Many of the investigations include testing and observation in the one person but with different alters. Different alter states have shown distinct physiological markers[12] and some EEG studies have shown distinct differences between alters in some subjects,[13][14] while other subjects' patterns were consistent across alters.[15] Another study concluded that the differences involved intensity of concentration, mood changes, degree of muscle tension, and duration of recording, rather than some inherent difference between the brains of people diagnosed with DID.[16] Brain imaging studies have corroborated the transitions of identity in some DID sufferers.[17] A link between epilepsy and DID has been postulated but this is disputed.[18][19] Some brain imaging studies have shown differing cerebral blood flow with different alters,[20][21][22] and distinct differences overall between subjects with DID and a healthy control group.[23] A different imaging study showed that findings of smaller hippocampal volumes in patients with a history of exposure to traumatic stress and an accompanying stress-related psychiatric disorder were also demonstrated in DID.[24] This study also found smaller amygdala volumes. Studies have demonstrated various changes in visual parameters between alters.[25][26][27] One twin study showed hereditable factors were present in DID.[28]
Causes
This disorder is theoretically linked with the interaction of overwhelming stress, traumatic antecedents,[29] insufficient childhood nurturing, and an innate ability to dissociate memories or experiences from consciousness.[9] A high percentage of patients report child abuse.[30][5] People diagnosed with DID often report that they have experienced severe physical and sexual abuse, especially during their childhood.[31] Several psychiatric rating scales of DID sufferers suggested that DID is strongly related to childhood trauma rather than to an underlying electrophysiological dysfunction.[32]
Others believe that the symptoms of DID are created iatrogenically by therapists using certain treatment techniques with suggestible patients,[2][4][5][6] but this idea is not universally accepted.[30][33][34][35][36][37] Skeptics have observed that a small number of therapists are responsible for diagnosing the majority of individuals with DID; that patients do not report sexual abuse or manifest alters until after treatment has begun; and the alternative explanation of the "alters" being rule-governed social roles rather than separate personalities.[6]
Development theory
It has been theorized that severe sexual, physical, or psychological trauma in childhood predisposes an individual to the development of DID. The steps in the development of a dissociative identity are theorized to be as follows:
- The child is harmed by a trusted caregiver (often a parent or guardian) and splits off the awareness and memory of the traumatic event to survive in the relationship.
- The memories and feelings go into the subconscious and are experienced later in the form of a separate personality.
- The process happens repeatedly at different times so that different personalities develop, containing different memories and performing different functions that are helpful or destructive.
- Dissociation becomes a coping mechanism for the individual when faced with further stressful situations.[38]
Diagnosis
The diagnosis of Dissociative identity disorder is defined by criteria in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM). The DSM-II used the term multiple personality disorder, the DSM-III grouped the diagnosis with the other four major dissociative disorders, and the DSM-IV-TR categorizes it as dissociative identity disorder. The ICD-10 continues to list the condition as multiple personality disorder.
The diagnostic criteria in section 300.14 (dissociative disorders) of the DSM-IV require that an adult, for non-physiological reasons, be recurrently controlled by multiple discrete identity or personality states while also suffering extensive memory lapses.[39] While otherwise similar, the diagnostic criteria for children requires also ruling out fantasy.
Diagnosis should be performed by a psychiatrist or psychologist who may use specially designed interviews (such as the SCID-D) and personality assessment tools to evaluate a person for a dissociative disorder.[1]
The psychiatric history of individuals diagnosed with DID frequently contain multiple previous diagnoses of various mental disorders and treatment failures.
Screening
The SCID-D[40] may be used to make a diagnosis. This interview takes about 30 to 90 minutes depending on the subject's experiences.
The Dissociative Disorders Interview Schedule (DDIS)[41] is a highly structured interview which discriminates between various DSM-IV diagnoses. The DDIS can usually be administered in 30–45 minutes.
The Dissociative Experiences Scale (DES)[42] is a simple, quick, and validated[43] questionnaire that has been widely used to screen for dissociative symptoms. Tests such as the DES provide a quick method of screening subjects so that the more time-consuming structured clinical interview can be used in the group with high DES scores. Depending on where the cutoff is set, people who would subsequently be diagnosed can be missed. An early recommended cutoff was 15-20[44] and in one study a DES with a cutoff of 30 missed 46 percent of the positive SCID-D[40] diagnoses and a cutoff of 20 missed 25%.[45] The reliability of the DES in non-clinical samples has been questioned.[46] There is also a DES scale for children and DES scale for adolescents. One study argued that old and new trauma may interact, causing higher DID item test scores.[29]
Differential diagnoses
Conditions which may present with similar symptoms include borderline personality disorder, and the dissociative conditions of dissociative amnesia and dissociative fugue.[47] The clearest distinction is the lack of discrete formed personalities in these conditions. Malingering may also be considered, and schizophrenia, although those with this last condition will have some form of delusions, hallucinations or thought disorder.[47]
Treatment
Treatment of DID may attempt to reconnect the identities of disparate alters into a single functioning identity. In addition or instead, treatment may focus on symptoms, to relieve the distressing aspects of the condition and ensure the safety of the individual. Treatment methods may include psychotherapy and medications for comorbid disorders.[1] Some behavior therapists initially use behavioral treatments such as only responding to a single identity, and using more traditional therapy once a consistent response is established.[48] It has been stated that treatment recommendations that follow from models that do not believe in the traumatic origins of DID might be harmful due to the fact that they ignore the posttraumatic symptomatology of people with DID.[35]
Prognosis
DID does not resolve spontaneously, and symptoms vary over time. Individuals with primarily dissociative symptoms and features of posttraumatic stress disorder normally recover with treatment. Those with comorbid addictions, personality, mood, or eating disorders face a longer, slower, and more complicated recovery process. Individuals still attached to abusers face the poorest prognosis; treatment may be long-term and consist solely of symptom relief rather than personality integration. Changes in identity, loss of memory, and awaking in unexplained locations and situations often leads to chaotic personal lives.[9] Individuals with the condition commonly attempt suicide.[49]
Epidemiology
The DSM does not provide an estimate of incidence; however the number of diagnoses of this condition has risen sharply. A possible explanation for the increase in incidence and prevalence of DID over time is that the condition was misdiagnosed as schizophrenia, bipolar disorder, or other such disorders in the past; another explanation is that an increase in awareness of DID and child sexual abuse has led to earlier, more accurate diagnosis. Other clinicians believe that DID is an iatrogenic condition overdiagnosed in highly suggestive individuals,[50] though there is disagreement over the ability of the condition to be induced by hypnosis.[33][34] Figures from psychiatric populations (inpatients and outpatients) show a wide diversity from different countries:[51]
| Country | Prevalence in mentally ill populations | Source study |
|---|---|---|
| India | 0.015% | Adityanjee et al. (1989)[52] |
| Switzerland | 0.05-0.1% | Modestin (1992)[53] |
| China | 0.4% | Xiao et al. (2006)[54] |
| Germany | 0.9% | Gast et al. (2001)[55] |
| The Netherlands | 2% | Friedl & Draijer (2000)[56] |
| U.S. | 10% | Bliss & Jeppsen (1985)[57] |
| U.S. | 6-8% | Ross et al. (1992)[58] |
| U.S. | 6-10% | Foote et al. (2006)[45] |
| Turkey | 14% | Sar et al. (2007)[59] |
Figures from the general population show less diversity:
| Country | Prevalence | Source study |
|---|---|---|
| Canada | 1% | Ross (1991)[60] |
| Turkey (male) | 0.4% | Akyuz et al. (1999)[61] |
| Turkey (female) | 1.1% | Sar et al. (2007)[62] |
Dissociative identity disorder is diagnosed in a sizable minority of patients in drug abuse treatment facilities.[5]
Comorbidity
Multiple identity disorder frequently co-occurs with other psychiatric diagnoses, such as anxiety disorders (especially post-traumatic stress disorder-PTSD), mood disorders, somatoform disorders, eating disorders, as well as sleep problems and sexual dysfunction.[49] The symptoms of the disorder have a considerable overlap with borderline personality disorder.[49]
History

Before the 19th century, people exhibiting symptoms similar to those were believed to be possessed.[49]
An intense interest in spiritualism, parapsychology, and hypnosis continued throughout the 19th and early 20th centuries,[8] running in parallel with John Locke's views that there was an association of ideas requiring the coexistence of feelings with awareness of the feelings.[63] Hypnosis, which was pioneered in the late 1700s by Franz Mesmer and Armand-Marie Jacques de Chastenet, Marques de Puységur, challenged Locke's association of ideas. Hypnotists reported what they thought were second personalities emerging during hypnosis and wondered how two minds could coexist.[8]
The 19th century saw a number of reported cases of multiple personalities which Rieber[63] estimated would be close to 100. Epilepsy was seen as a factor in some cases,[63] and discussion of this connection continues into the present era.[15][18]
By the late 19th century there was a general acceptance that emotionally traumatic experiences could cause long-term disorders which may manifest with a variety of symptoms.[64] These conversion disorders were found to occur in even the most resilient individuals, but with profound effect in someone with emotional instability like Louis Vivé (1863-?) who suffered a traumatic experience as a 13 year-old when he encountered a viper. Vivé was the subject of countless medical papers and became the most studied case of dissociation in the 19th century.
Between 1880 and 1920, many great international medical conferences devoted a lot of time to sessions on dissociation.[65] It was in this climate that Jean-Martin Charcot introduced his ideas of the impact of nervous shocks as a cause for a variety of neurological conditions. One of Charcot's students, Pierre Janet, took these ideas and went on to develop his own theories of dissociation.[66] One of the first individuals diagnosed with multiple personalities to be scientifically studied was Clara Norton Fowler, under the pseudonym Christine Beauchamp; American neurologist Morton Prince studied Fowler between 1898 and 1904, describing her case study in his 1906 monograph, Dissociation of a Personality.[66] Fowler went on to marry one of her analyst's colleagues.[67]
In the early 20th century interest in dissociation and multiple personalities waned for a number of reasons. After Charcot's death in 1893, many of his so-called hysterical patients were exposed as frauds, and Janet's association with Charcot tarnished his theories of dissociation.[8] Sigmund Freud recanted his earlier emphasis on dissociation and childhood trauma.[8]
In 1910, Eugen Bleuler introduced the term schizophrenia to replace dementia praecox. A review of the Index medicus from 1903 through 1978 showed a dramatic decline in the number of reports of multiple personality after the diagnosis of schizophrenia became popular, especially in the United States.[68] A number of factors helped create a large climate of skepticism and disbelief; paralleling the increased suspicion of DID was the decline of interest in dissociation as a laboratory and clinical phenomenon.[65]
Starting in about 1927, there was a large increase in the number of reported cases of schizophrenia, which was matched by an equally large decrease in the number of multiple personality reports.[65] Bleuler also included multiple personality in his category of schizophrenia. It was concluded in the 1980s that DID patients are often misdiagnosed as suffering from schizophrenia.[65]
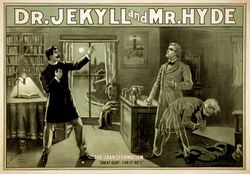
The public, however, was exposed to psychological ideas which took their interest. Mary Shelley's Frankenstein, Robert Louis Stevenson's Strange Case of Dr Jekyll and Mr Hyde, and many short stories by Edgar Allan Poe had a formidable impact.[63] In 1957, with the publication of the book The Three Faces of Eve and the popular movie which followed it, the American public's interest in multiple personality was revived. During the 1970s an initially small number of clinicians campaigned to have it considered a legitimate diagnosis.[65]
Between 1968 and 1980 the term that was used for dissociative identity disorder was "Hysterical neurosis, dissociative type". The APA wrote: "In the dissociative type, alterations may occur in the patient's state of consciousness or in his identity, to produce such symptoms as amnesia, somnambulism, fugue, and multiple personality."[69]
The highly influential book Sybil was published in 1974, which popularized the diagnosis through a detailed discussion of the problems and treatment of the pseudonymous Sybil. Six years later, the diagnosis of multiple personality disorder appeared in the DSM III.[49] Controversy over the iconic case has since arisen, with some calling Sybil's diagnosis the result of iatrogenic therapeutic methods[70] while others have defended the treatment and reputation of Sybil's therapist, Cornelia B. Wilbur.[71] As media coverage spiked, diagnoses climbed. There were 200 reported cases of DID as of 1980, and 20,000 from 1980 to 1990.[72] Joan Acocella reports that 40,000 cases were diagnosed from 1985 to 1995.[73] The majority of diagnoses are made in North America, particularly the United States, and in English-speaking countries more generally[74] with reports recently emerging from other countries.[52][53][54][55][56][59][61]
Society and culture
Controversy
DID is a controversial diagnosis and condition, with much of the literature on DID being generated and published in North America, to the extent that it was regarded as a phenomenon confined to that continent.[8][2] Even among North American psychiatrists there is a lack of consensus regarding the validity of DID.[3][75] Practitioners who do accept DID as a valid disorder have produced an extensive literature with some of the more recent papers originating outside North America.[76] Criticism of the diagnosis continues, with Piper and Merskey describing it as a culture-bound and often iatrogenic condition which they believe is in decline.[2][4] There is considerable controversy over the validity of the multiple personality profile as a diagnosis. Unlike the more empirically verifiable mood and personality disorders, dissociation is primarily subjective for both the patient and the treatment provider. The relationship between dissociation and multiple personality creates conflict regarding the DID diagnosis. While other disorders require a certain amount of subjective interpretation, those disorders more readily present generally accepted, objective symptoms. The controversial nature of the dissociation hypothesis is shown quite clearly by the manner in which the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) has addressed, and re-addressed, the categorization over the years.
The second edition of the DSM referred to this diagnostic profile as multiple personality disorder. The third edition grouped MPD in with the other four major dissociative disorders. The current edition, the DSM-IV-TR, categorizes the disorder as dissociative identity disorder (DID). The ICD-10 (International Statistical Classification of Diseases and Related Health Problems) continues to list the condition as multiple personality disorder.
Psychiatrist Colin A. Ross has stated that based on documents obtained through freedom of information legislation, psychiatrists linked to Project MKULTRA claimed to be able to to deliberately induce dissociative identity disorder using a variety of aversive techniques.[77]
Over-representation in North America
In a review,[7] Joel Paris offered three possible causes for the sudden increase in people diagnosed with DID:
- The result of therapist suggestions to suggestible people, much as Charcot's hysterics acted in accordance with his expectations.
- Psychiatrists' past failure to recognize dissociation being redressed by new training and knowledge.
- Dissociative phenomena are actually increasing, but this increase only represents a new form of an old and protean entity: "hysteria".
Paris believes that the first possible cause is the most likely.
The debate over the validity of this condition, whether as a clinical diagnosis, a symptomatic presentation, a subjective misrepresentation on the part of the patient, or a case of unconscious collusion on the part of the patient and the professional is considerable. There are several main points of disagreement over the diagnosis.
Skeptics claim that people who present with the appearance of alleged multiple personality may have learned to exhibit the symptoms in return for social reinforcement. One case cited as an example for this viewpoint is the "Sybil" case, popularized by the news media. Psychiatrist Herbert Spiegel stated that "Sybil" had been provided with the idea of multiple personalities by her treating psychiatrist, Cornelia Wilbur, to describe states of feeling with which she was unfamiliar.
One of the primary reasons for the ongoing recategorization of this condition is that there were once so few documented cases (research in 1944 showed only 76[78]) of what was once referred to as multiple personality. Dissociation is recognized as a symptomatic presentation in response to trauma, extreme emotional stress, and, as noted, in association with emotional dysregulation and borderline personality disorder.[79]
See also
- Dissociation
- Fugue state
- Identity formation
- Psychogenic amnesia
- Splitting (psychology)
- Dissociative identity disorder in popular culture
- Session 9
Footnotes
- ↑ 1.0 1.1 1.2 "Mental Health: Dissociative Identity Disorder (Multiple Personality Disorder)". Webmd.com. http://www.webmd.com/content/article/118/112901.htm. Retrieved 2007-12-10.
- ↑ 2.0 2.1 2.2 2.3 2.4 Piper A, Merskey H (2004). "The persistence of folly: a critical examination of dissociative identity disorder. Part I. The excesses of an improbable concept" (pdf). Canadian journal of psychiatry. Revue canadienne de psychiatrie 49 (9): 592–600. PMID 15503730. http://ww1.cpa-apc.org:8080/Publications/Archives/CJP/2004/september/piper.pdf.
- ↑ 3.0 3.1 Pope HG, Oliva PS, Hudson JI, Bodkin JA, Gruber AJ (1999). "Attitudes toward DSM-IV dissociative disorders diagnoses among board-certified American psychiatrists". The American journal of psychiatry 156 (2): 321–3. PMID 9989574.
- ↑ 4.0 4.1 4.2 Piper A, Merskey H (2004). "The persistence of folly: critical examination of dissociative identity disorder. Part II. The defence and decline of multiple personality or dissociative identity disorder". Canadian journal of psychiatry. Revue canadienne de psychiatrie 49 (10): 678–83. PMID 15560314. Full Text
- ↑ 5.0 5.1 5.2 5.3 "Dissociative Identity Disorder, patient's reference". Merck.com. 2003-02-01. http://www.merck.com/mmhe/sec07/ch106/ch106e.html. Retrieved 2007-12-07.
- ↑ 6.0 6.1 6.2 Carroll, RT (2007-12-03). "Multiple personality disorder (dissociative identity disorder)". Skeptic’s Dictionary. http://www.skepdic.com/mpd.html. Retrieved 2008-01-22.
- ↑ 7.0 7.1 Paris J (1996). "Review-Essay : Dissociative Symptoms, Dissociative Disorders, and Cultural Psychiatry". Transcult Psychiatry 33 (1): 55–68. doi:10.1177/136346159603300104.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Atchison M, McFarlane AC (1994). "A review of dissociation and dissociative disorders". The Australian and New Zealand journal of psychiatry 28 (4): 591–9. doi:10.3109/00048679409080782. PMID 7794202.
- ↑ 9.0 9.1 9.2 9.3 "Dissociative Identity Disorder, doctor's reference". Merck.com. 2005-11-01. http://www.merck.com/mmpe/sec15/ch197/ch197e.html. Retrieved 2007-12-07.
- ↑ Putnam FW (1984). "The psychophysiologic investigation of multiple personality disorder. A review". Psychiatr. Clin. North Am. 7 (1): 31–9. PMID 6371727.
- ↑ Miller SD, Triggiano PJ (1992). "The psychophysiological investigation of multiple personality disorder: review and update". The American journal of clinical hypnosis 35 (1): 47–61. PMID 1442640.
- ↑ Putnam FW, Zahn TP, Post RM (1990). "Differential autonomic nervous system activity in multiple personality disorder". Psychiatry research 31 (3): 251–60. doi:10.1016/0165-1781(90)90094-L. PMID 2333357.
- ↑ Hughes JR, Kuhlman DT, Fichtner CG, Gruenfeld MJ (1990). "Brain mapping in a case of multiple personality". Clinical EEG (electroencephalography) 21 (4): 200–9. PMID 2225470.
- ↑ Lapointe AR, Crayton JW, DeVito R, Fichtner CG, Konopka LM (2006). "Similar or disparate brain patterns? The intra-personal EEG variability of three women with multiple personality disorder". Clinical EEG and neuroscience : official journal of the EEG and Clinical Neuroscience Society (ENCS) 37 (3): 235–42. PMID 16929711.
- ↑ 15.0 15.1 Cocores JA, Bender AL, McBride E (1984). "Multiple personality, seizure disorder, and the electroencephalogram". J. Nerv. Ment. Dis. 172 (7): 436–8. doi:10.1097/00005053-198407000-00011. PMID 6427406.
- ↑ Coons PM, Milstein V, Marley C (1982). "EEG studies of two multiple personalities and a control". Arch. Gen. Psychiatry 39 (7): 823–5. PMID 7165480.
- ↑ "Psychology Today's Diagnosis Dictionary Dissociative Identity Disorder (Multiple Personality Disorder)". New York, NY: Sussex Publishers LLC. October 2005. http://psychologytoday.com/conditions/did.html. Retrieved 2008-02-19.
- ↑ 18.0 18.1 Devinsky O, Putnam F, Grafman J, Bromfield E, Theodore WH (1989). "Dissociative states and epilepsy". Neurology 39 (6): 835–40. PMID 2725878.
- ↑ Ross CA, Heber S, Anderson G, et al. (1989). "Differentiating multiple personality disorder and complex partial seizures". General Hospital Psychiatry 11 (1): 54–8. doi:10.1016/0163-8343(89)90026-1. PMID 2912820.
- ↑ Reinders AA, Nijenhuis ER, Paans AM, Korf J, Willemsen AT, den Boer JA (2003). "One brain, two selves". Neuroimage 20 (4): 2119–25. doi:10.1016/j.neuroimage.2003.08.021. PMID 14683715.
- ↑ Reinders AA, Nijenhuis ER, Quak J, et al. (2006). "Psychobiological characteristics of dissociative identity disorder: A symptom provocation study". Biol. Psychiatry 60 (7): 730–40. doi:10.1016/j.biopsych.2005.12.019. PMID 17008145.
- ↑ Mathew RJ, Jack RA, West WS (1985). "Regional cerebral blood flow in a patient with split personality". The American Journal of Psychiatry 142 (4): 504–5. PMID 3976929.
- ↑ Sar V, Unal SN, Ozturk E (2007). "Frontal and occipital perfusion changes in dissociative identity disorder". Psychiatry Research 156 (3): 217–23. doi:10.1016/j.pscychresns.2006.12.017. PMID 17961993.
- ↑ Vermetten E, Schmahl C, Lindner S, Loewenstein RJ, Bremner JD (2006). "Hippocampal and amygdalar volumes in dissociative identity disorder". The American journal of psychiatry 163 (4): 630–6. doi:10.1176/appi.ajp.163.4.630. PMID 16585437.
- ↑ Miller SD (1989). "Optical differences in cases of multiple personality disorder". J. Nerv. Ment. Dis. 177 (8): 480–6. doi:10.1097/00005053-198908000-00005. PMID 2760599.
- ↑ Miller SD, Blackburn T, Scholes G, White GL, Mamalis N (1991). "Optical differences in multiple personality disorder. A second look". J. Nerv. Ment. Dis. 179 (3): 132–5. doi:10.1097/00005053-199103000-00003. PMID 1997659.
- ↑ Birnbaum MH, Thomann K (1996). "Visual function in multiple personality disorder". Journal of the American Optometric Association 67 (6): 327–34. PMID 8888853.
- ↑ Jang KL, Paris J, Zweig-Frank H, Livesley WJ (1998). "Twin study of dissociative ~~~~experience". J. Nerv. Ment. Dis. 186 (6): 345–51. doi:10.1097/00005053-199806000-00004. PMID 9653418.
- ↑ 29.0 29.1 Pearson, M.L. (1997). "Childhood trauma, adult trauma, and dissociation" (PDF). Dissociation 10 (1): 58–62:. https://scholarsbank.uoregon.edu/dspace/bitstream/1794/1837/1/Diss_10_1_9_OCR.pdf. Retrieved 2008-06-01.
- ↑ 30.0 30.1 Kluft, RP (2003). "Current Issues in Dissociative Identity Disorder" (PDF). Bridging Eastern and Western Psychiatry 1 (1): 71–87. http://www.psyter.org/allegati/180/Kluft.pdf. Retrieved 2008-05-09.
- ↑ American Psychiatric Association (2000-06). Diagnostic and Statistical Manual of Mental Disorders DSM-IV TR (Text Revision). Arlington, VA, USA: American Psychiatric Publishing, Inc.. p. 943. doi:10.1176/appi.books.9780890423349. ISBN 978-0890420249. http://www.psychiatryonline.com/resourceTOC.aspx?resourceID=1.
- ↑ Coons PM, Bowman ES, Milstein V. Multiple personality disorder. A clinical investigation of 50 cases. J Nerv Ment Dis. 1988 Sep;176(9):519-27
- ↑ 33.0 33.1 Braun, B.G. (1989) (PDF). Dissociation: Vol. 2, No. 2, p. 066-069: Iatrophilia and Iatrophobia in the diagnosis and treatment of MPD. https://scholarsbank.uoregon.edu/dspace/bitstream/1794/1425/1/Diss_2_2_3_OCR.pdf. Retrieved 2008-05-04.
- ↑ 34.0 34.1 Brown, D; Frischholz E, Scheflin A. (1999). "Iatrogenic dissociative identity disorder - an evaluation of the scientific evidence". The Journal of Psychiatry and Law XXVII No. 3-4 (Fall-Winter 1999): 549–637.
- ↑ 35.0 35.1 Gleaves, D. (July 1996). "The sociocognitive model of dissociative identity disorder: a reexamination of the evidence". Psychological Bulletin 120 (1): 42–59. doi:10.1037/0033-2909.120.1.42. PMID 8711016.
- ↑ Ross, C.; Norton, G. & Fraser, G. (1989). "Evidence against the iatrogenesis of multiple personality disorder" (PDF). Dissociation 2 (2): 61–65. https://scholarsbank.uoregon.edu/dspace/bitstream/1794/1424/1/Diss_2_2_2_OCR.pdf. Retrieved 2008-02-10.
- ↑ Kluft, R.P. (1989). "Iatrongenic creation of new alter personalities" (PDF). Dissociation 2 (2): 83–91. https://scholarsbank.uoregon.edu/dspace/bitstream/1794/1428/1/Diss_2_2_6_OCR.pdf. Retrieved 2008-04-21.
- ↑ Carson VB; Shoemaker, NC & Varcarolis E. Foundations of Psychiatric Mental Health Nursing: A Clinical Approach (5 ed.). St. Louis: Saunders Elsevier. pp. 266–267. ISBN 1-4160-0088-7.
- ↑ American Psychiatric Association (2000). "Diagnostic criteria for 300.14 Dissociative Identity Disorder". Diagnostic and Statistical Manual of Mental Disorders (4th, text revision (DSM-IV-TR) ed.). ISBN 0-89042-025-4. http://behavenet.com/capsules/. Retrieved 2010-03-14.
- ↑ 40.0 40.1 Steinberg M, Rounsaville B, Cicchetti DV (1990). "The Structured Clinical Interview for DSM-III-R Dissociative Disorders: preliminary report on a new diagnostic instrument". The American journal of psychiatry 147 (1): 76–82. PMID 2293792.
- ↑ Ross CA, Ellason JW (2005). "Discriminating among diagnostic categories using the Dissociative Disorders Interview Schedule". Psychological reports 96 (2): 445–53. doi:10.2466/PR0.96.2.445-453. PMID 15941122.
- ↑ Bernstein EM, Putnam FW (1986). "Development, reliability, and validity of a dissociation scale". J. Nerv. Ment. Dis. 174 (12): 727–35. doi:10.1097/00005053-198612000-00004. PMID 3783140.
- ↑ Carlson EB, Putnam FW, Ross CA, et al. (1993). "Validity of the Dissociative Experiences Scale in screening for multiple personality disorder: a multicenter study". The American journal of psychiatry 150 (7): 1030–6. PMID 8317572.
- ↑ Steinberg M, Rounsaville B, Cicchetti D (1991). "Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured diagnostic interview". The American journal of psychiatry 148 (8): 1050–4. PMID 1853955.
- ↑ 45.0 45.1 Foote B, Smolin Y, Kaplan M, Legatt ME, Lipschitz D (2006). "Prevalence of dissociative disorders in psychiatric outpatients". The American journal of psychiatry 163 (4): 623–9. doi:10.1176/appi.ajp.163.4.623. PMID 16585436. Full Text
- ↑ Wright DB, Loftus EF (1999). "Measuring dissociation: comparison of alternative forms of the dissociative experiences scale". The American journal of psychology (The American Journal of Psychology, Vol. 112, No. 4) 112 (4): 497–519. doi:10.2307/1423648. PMID 10696264. http://jstor.org/stable/1423648. Page 1
- ↑ 47.0 47.1 Sadock 2002, p. 683
- ↑ Kohlenberg, R.J.; Tsai, M. (1991). Functional Analytic Psychotherapy: Creating Intense and Curative Therapeutic Relationships. Springer. ISBN 0306438577.
- ↑ 49.0 49.1 49.2 49.3 49.4 Sadock 2002, p. 681
- ↑ American Psychiatric Association (2000-06). Diagnostic and Statistical Manual of Mental Disorders DSM-IV TR (Text Revision). Arlington, VA, USA: American Psychiatric Publishing, Inc.. pp. 526–528. doi:10.1176/appi.books.9780890423349. ISBN 978-0890420249.
- ↑ Boon S, Draijer N (1991). "Diagnosing dissociative disorders in The Netherlands: a pilot study with the Structured Clinical Interview for DSM-III-R Dissociative Disorders". The American journal of psychiatry 148 (4): 458–62. PMID 2006691.
- ↑ 52.0 52.1 Adityanjee, Raju GS, Khandelwal SK (1989). "Current status of multiple personality disorder in India". The American journal of psychiatry 146 (12): 1607–10. PMID 2589555.
- ↑ 53.0 53.1 Modestin J (1992). "Multiple personality disorder in Switzerland". The American journal of psychiatry 149 (1): 88–92. PMID 1728191.
- ↑ 54.0 54.1 Xiao Z, Yan H, Wang Z, et al. (2006). "Trauma and dissociation in China". The American journal of psychiatry 163 (8): 1388–91. doi:10.1176/appi.ajp.163.8.1388. PMID 16877651.
- ↑ 55.0 55.1 Gast U, Rodewald F, Nickel V, Emrich HM (2001). "Prevalence of dissociative disorders among psychiatric inpatients in a German university clinic". J. Nerv. Ment. Dis. 189 (4): 249–57. doi:10.1097/00005053-200104000-00007. PMID 11339321.
- ↑ 56.0 56.1 Friedl MC, Draijer N (2000). "Dissociative disorders in Dutch psychiatric inpatients". The American journal of psychiatry 157 (6): 1012–3. doi:10.1176/appi.ajp.157.6.1012. PMID 10831486.
- ↑ Bliss EL, Jeppsen EA (1985). "Prevalence of multiple personality among inpatients and outpatients". The American journal of psychiatry 142 (2): 250–1. PMID 3970252.
- ↑ Ross CA, Anderson G, Fleisher WP, Norton GR (1992). "Dissociative experiences among psychiatric inpatients". General hospital psychiatry 14 (5): 350–4. doi:10.1016/0163-8343(92)90071-H. PMID 1521791.
- ↑ 59.0 59.1 Sar V, Koyuncu A, Ozturk E, et al. (2007). "Dissociative disorders in the psychiatric emergency ward". General hospital psychiatry 29 (1): 45–50. doi:10.1016/j.genhosppsych.2006.10.009. PMID 17189745.
- ↑ Ross CA (1991). "Epidemiology of multiple personality disorder and dissociation". Psychiatr. Clin. North Am. 14 (3): 503–17. PMID 1946021.
- ↑ 61.0 61.1 Akyüz G, Doğan O, Sar V, Yargiç LI, Tutkun H (1999). "Frequency of dissociative identity disorder in the general population in Turkey". Comprehensive psychiatry 40 (2): 151–9. doi:10.1016/S0010-440X(99)90120-7. PMID 10080263.
- ↑ Sar V, Akyüz G, Doğan O (2007). "Prevalence of dissociative disorders among women in the general population". Psychiatry Res 149 (1-3): 169–76. doi:10.1016/j.psychres.2006.01.005. PMID 17157389.
- ↑ 63.0 63.1 63.2 63.3 Rieber RW (2002). "The duality of the brain and the multiplicity of minds: can you have it both ways?". History of psychiatry 13 (49 Pt 1): 3–17. doi:10.1177/0957154X0201304901. PMID 12094818.
- ↑ Borch-Jacobsen M, Brick D (2000). "How to predict the past: from trauma to repression". History of Psychiatry 11 (41 Pt 1): 15–35. doi:10.1177/0957154X0001104102. PMID 11624606.
- ↑ 65.0 65.1 65.2 65.3 65.4 Putnam, Frank W. (1989). Diagnosis and Treatment of Multiple Personality Disorder. New York: The Guilford Press. pp. 351. ISBN 0-89862-177-1.
- ↑ 66.0 66.1 van der Kolk BA, van der Hart O (December 1989). "Pierre Janet and the breakdown of adaptation in psychological trauma". Am J Psychiatry 146 (12): 1530–40. PMID 2686473. http://ajp.psychiatryonline.org/cgi/pmidlookup?view=long&pmid=2686473.
- ↑ Bethune, B (2007-11-26). "What drove women mad?". Maclean's (Rogers Communications). http://www.macleans.ca/culture/lifestyle/article.jsp?content=20071115_98997_98997. Retrieved 2009-02-18.
- ↑ Rosenbaum M (1980). "The role of the term schizophrenia in the decline of diagnoses of multiple personality". Arch. Gen. Psychiatry 37 (12): 1383–5. PMID 7004385.
- ↑ American Psychiatric Association. 1968. Hysterical Neurosis. Diagnostic and statistical manual of mental disorders second edition pg 40. Washington, D.C.
- ↑ Rieber, R (1999). "Hypnosis, false memory and multiple personality: a trinity of affinity". History of Psychiatry 10 (37): 3–11. doi:10.1177/0957154X9901003701. PMID 11623821.
- ↑ Ritter, M (1998-08-16). "Doubt Cast on Story of 'Sybil'". Associated Press.
- ↑ Adams, C (2003). "Does multiple personality disorder really exist?". The Straight Dope. http://www.straightdope.com/columns/031003.html. Retrieved 2008-01-22.
- ↑ Acocella, JR (1999). Creating hysteria: Women and multiple personality disorder. San Francisco: Jossey-Bass Publishers. ISBN 0-7879-4794-6.
- ↑ Spanos, Nicholas P. (1996). Multiple Identities & False Memories: A Sociocognitive Perspective. American Psychological Association (APA). ISBN 1557983402.
- ↑ Lalonde JK, Hudson JI, Gigante RA, Pope HG (2001). "Canadian and American psychiatrists' attitudes toward dissociative disorders diagnoses". Canadian journal of psychiatry. Revue canadienne de psychiatrie 46 (5): 407–12. PMID 11441778.
- ↑ Rhoades, G. F., Sar, V. (editors) (2006) Trauma And Dissociation in a Cross-cultural Perspective: Not Just a North American Phenomenon. Routledge. ISBN 978-0-7890-3407-6
- ↑ Ross, C (2000). Bluebird: Deliberate Creation of Multiple Personality Disorder by Psychiatrists. Manitou Communications. ISBN 978-0970452511.
- ↑ "Creating Hysteria by Joan Acocella". The New York Times. 1999. http://www.nytimes.com/books/first/a/acocella-hysteria.html.
- ↑ Marmer S, Fink D (1994). "Rethinking the comparison of Borderline Personality Disorder and multiple personality disorder". Psychiatr Clin North Am 17 (4): 743–71. PMID 7877901.
References
- Sadock, Benjamin J.; Sadock, Virginia A. (2002). Kaplan and Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (9th ed.). Lippincott Williams & Wilkins. ISBN 0781731836.
Further reading
- Goettmann, B. A.; Greaves BG; Coons MP (1994). Multiple personality and dissociation, 1791-1992: a complete bibliography. Lutherville, MD: The Sidran Press. pp. 85. ISBN 0-9629164-5-5. http://boundless.uoregon.edu/cdm4/item_viewer.php?CISOROOT=/diss&CISOPTR=38.
External links
- Dissociative identity disorder at the Open Directory Project
- International Society for the Study of Trauma and Dissociation
- Multiple Personality Disorder entry at The Skeptic's Dictionary
- A brain imaging project on dissociative identity disorder
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||